- The HNS CPR Program is based on the core tenet that physicians should be able to make treatment decisions based upon their own clinical judgments and does not include medical necessity determinations. The program does not mandate the number or type of services physicians may provide nor the frequency or length of time in which treatment may be provided. CPRs are statistical reviews of the network's and individual physician's performance relative to costs and practice patterns.
- The program is designed to improve cost-efficiency by regularly providing meaningful and actionable cost and utilization data to the physicians in the HNS Network.
- Through the use of performance-based tiers, recognition programs, and administrative withholds, the CPR Program aligns incentives and rewards the delivery of cost-efficient care.
- The metrics utilized in the CPR Program, against which physician performance is measured, are based on the collective costs and practice patterns of the physicians in the HNS network.
- The CPR Program includes the establishment of target performance goals relative to cost-efficiency for the individual physician and for the network as a whole.
- HNS evaluates the physician's and the network's aggregate performance against these goals. The program includes annual and monthly performance reviews.
- The program utilizes the "average cost per patient" as the primary metric to evaluate physician and network performance for cost-efficiency.
- Because the network's actual "average cost per patient" may fluctuate, to ensure fair and appropriate performance measurement, a target "average cost per patient" benchmark is established at the beginning of each calendar year and is used throughout the year. The target benchmark may increase each year, but will not decrease.
- For the target benchmark, HNS utilizes the higher of the actual network average obtained using a trimmed mean approach OR the highest actual network average from the previous five years.
- CPRs compare the physician's average cost per patient to the target benchmark.
- Variations in types of practices ("specialty" practices), patient demographics, clinical characteristics, co-morbidities, responses to treatment, etc., all impact a physician's "average cost per patient". To appropriately allow for these variations when measuring physician performance, the CPR Program utilizes a range of acceptance (ROA) from the target benchmark.
- HNS conducts an annual review of average "case costs" (using primary diagnoses) to ensure the HNS ROA appropriately accommodates those costs.
- In January of each year, HNS conducts an annual review of physician and network performance relative to cost-efficiency. Annual reviews reflect performance based on data from claims submitted through HNS during the previous calendar year.
- Based on the physician's "average cost per patient" and the relationship of his/her "average cost per patient" to the HNS target benchmark, HNS assigns a performance measurement ("plan ranking") to each physician, for each health care plan reviewed.
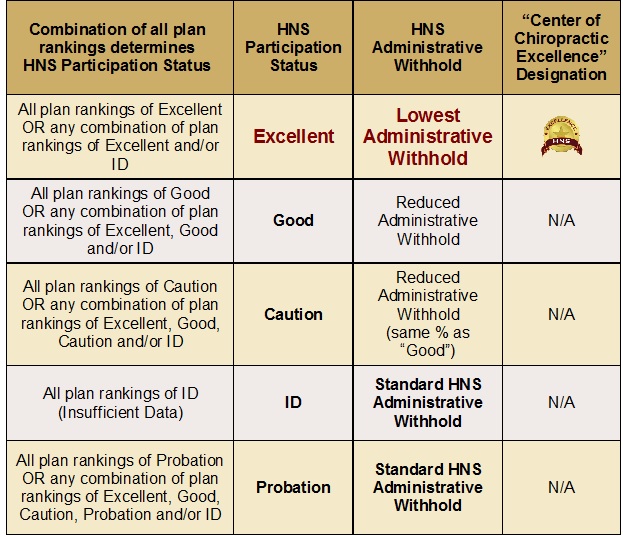
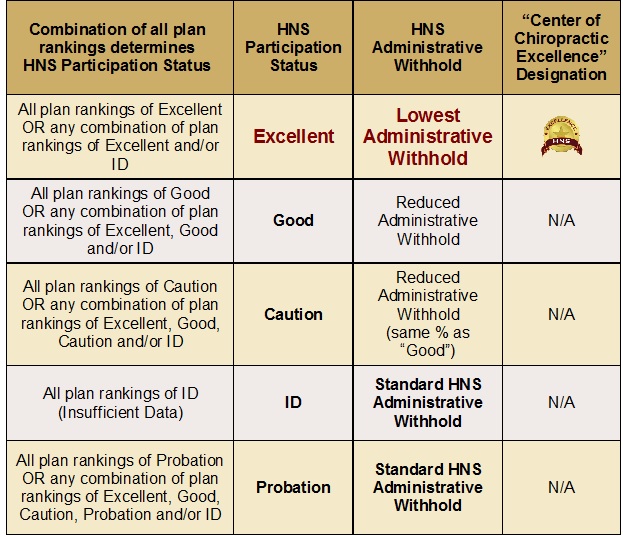
- The combination of "plan rankings" from the annual review determines each physician's HNS Participation Status. The participation status assigned to each physician is based on the lowest plan ranking for the review period. With a few exceptions, the physician's HNS Participation Status determines his/her HNS Administrative Withhold for the remainder of the calendar year and the HNS Participation Status cannot be changed until the next annual review.
- When measuring performance, average costs per patient within 151% of the HNS benchmark are considered indicative of cost-effective care, while average costs per patient in excess of 151% indicate sub-optimal performance, and result in probationary status.
Plan rankings and participation status include:
Excellent - Avg. cost per patient is within 115% (within ROA);
Good - Avg. cost per patient is between 115% and 141% (within ROA);
Caution - Avg. cost per patient is between 141% and 151% (within ROA);
Probation - Avg. cost per patient is greater than 151% (exceeds ROA);
ID - indicates insufficient data to gauge cost-effectiveness. Performance measurements of ID indicate there is insufficient data for the specific review period, relative to a particular health care plan, to gauge cost-effectiveness. Plan rankings of ID, as a general rule, do not negatively impact a physician. However, close attention should be paid to a plan ranking of ID, as this ranking will change as soon as there is a sufficient amount of data to gauge cost-effectiveness. To alert the physician to what his/her plan ranking would have been had the data threshold been met for the review period, HNS assigns a sub-classification to plan rankings of ID. This sub-classification represents the variation from the physician's average cost per patient to the HNS target benchmark for the specific health care plan, for the specific review period.
- Results of the annual review are provided via the HNS Comparative Practice Patterns Report (CPR). CPRs include the physician's "average cost per patient", compares the physician's "average cost per patient" to the HNS benchmark and range of acceptance for this metric, displays the physician's plan ranking for each health plan, the HNS Participation Status, and the HNS Administrative Withhold.
- Top performers (those physicians whose average costs per patient are within 115% of the HNS target benchmark) are generally rewarded via a reduction to their HNS Administrative Withhold and receive special recognition as an "HNS Center of Excellence" in the HNS online physician directory.

This designation is published with the physician's name in the HNS Provider Directory and is designed to improve transparency, allowing members to make better-informed health care decisions and may promote steerage to the most cost-efficient physicians.
The table below is an example of how various plan rankings and HNS admin fees may be impacted by Participation Status.
- In addition to the annual review, HNS conducts monthly performance reviews. With few exceptions, each monthly review is based on the most recent 12 months of claims data. If any monthly review indicates underperformance, the physician's participation status may be changed to probation.
- Because there may be circumstances in which the assigned participation status is not appropriate, physicians have the right to appeal their HNS Participation Status within 30 days of the date the HNS Participation Status is first assigned. However, if a physician chooses not to appeal his status, HNS concludes the physician does not dispute the assigned participation status, and understands that termination may occur, if applicable, should performance not improve within the specified period.
- Because continued participation in the HNS network requires the consistent delivery of effective, cost-efficient care, physicians whose practice patterns are inconsistent with cost-efficient care, as defined by CPR Program parameters, are placed on Probationary Status for a period of 12 months.
- Providers on probation are offered peer-to peer counseling from one of the HNS Chiropractic Medical Directors, are provided a specific time frame to improve cost-efficiency and are required to successfully complete six hours of a specified continuing education course designed to help improve treatment outcomes and cost-efficiency.
- To ensure a probationary provider's performance is measured fairly during the 12 month probationary period, HNS only reviews data from claims submitted since the onset of the probationary period. HNS generates "interim" CPR reports for the provider each month of the probationary period, the provider's "average cost per patient" is compared to the actual HNS network average for the specific reporting period.
- While significant efforts will be made to assist physicians in improving cost-efficiency, generally speaking, physicians whose average costs per patient are not consistent with cost-efficient care, as defined by CPR Program parameters, within the time frames established to demonstrate improvement, and who do not appeal their participation status, face termination of their participation in the network.
- In most instances, physicians have the right to appeal CPR decisions to terminate their participation in the network. If a physician appeals either the participation status determination or the termination decision, the physician must submit a notice of appeal, in writing, to HNS. As part of the review process, HNS may review copies of a number of the physician's health care records for compliance to HNS and contracted health care plan policies.
|
 Health Network Solutions, Inc. (HNS) stands alone as the oldest and largest chiropractic network in the Southeast.
Health Network Solutions, Inc. (HNS) stands alone as the oldest and largest chiropractic network in the Southeast.